Chronic otitis media
Following an attack of acute otitis the perforation and discharge may persist – chron- ic otitis media. This leads to mixed infection and further damage to the middle-ear structures, with worsening conductive deafness. The predisposing factors in the de- velopment of chronic otitis media are listed in Box 9.1. Suppuration with discharge-chronic suppurative otitis media (CSOM) – can be further classified as in Box 9.2.
Box 9.1 Causes of chronic otitis media
1 Late or inadequate treatment of acute otitis media.
2 Upper airway sepsis.
3 Lowered resistance, e.g. malnutrition, anaemia, immunological impairment.
1 Late or inadequate treatment of acute otitis media.
2 Upper airway sepsis.
3 Lowered resistance, e.g. malnutrition, anaemia, immunological impairment.
Box 9.2 Types of CSOM
1 Mucosal disease with tympanic membrane perforation (relatively safe).
2 Bony:
a Osteitis.
b Cholesteatoma – an epithelial sac which erodes the middle ear and adjacent structures including the meninges.
1 Mucosal disease with tympanic membrane perforation (relatively safe).
2 Bony:
a Osteitis.
b Cholesteatoma – an epithelial sac which erodes the middle ear and adjacent structures including the meninges.
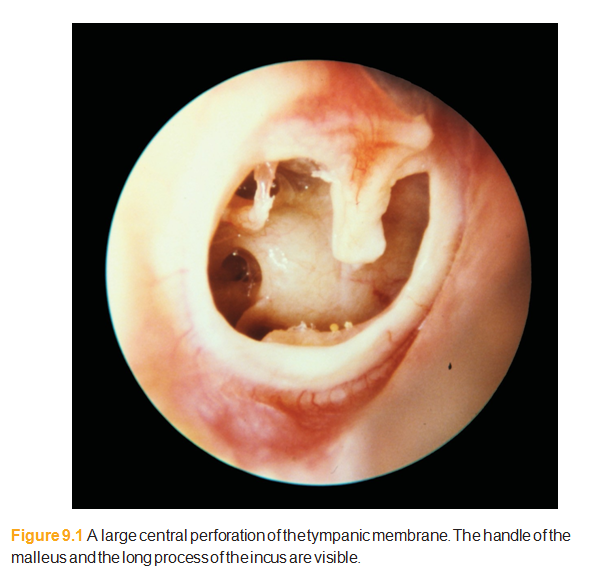
The perforated ear
A perforated eardrum may be asymptomatic. If unilateral, the relatively minor conductive hearing loss causes little or no trouble. The ear may discharge during an upper respiratory infection or if it becomes contaminated by water, e.g. after swimming. Some patients have persistent mucosal infection (active CSOM). In these cases there may be underlying nasal or pharyngeal sepsis that will require attention if the ear is to heal. The ear will discharge, usually copiously, and the dis- charge is mucoid. The perforation may be large (Fig. 9.1) or very small and difficult to see. A short course of antibiotic eardrops can help dry up a discharging ear but many proprietary preparations contain aminoglycosides which can cause deaf- ness. Ciprofloxacin is better. Systemic antibiotics are of little use. There is no point in persisting with prolonged courses of topical antibiotics. The mainstay of treat- ment is thorough and regular aural toilet. A small perforation may heal. Persistent infection can cause erosion of bone (bony CSOM) and eventually infection can spread beyond the ear, e.g. intracranial. Serious complications are very rare but if left untreated the condition may result in permanent deafness or intracranial sepsis. If squamous epithelium collects in the middle ear (cholesteatoma) it can erode adjacent structures and cause serious complications. Surgery is usually needed to manage cholesteatoma.
Myringoplasty
When there is a dry perforation, surgery may be considered but is not manda- tory. Myringoplasty is the repair of a tympanic membrane perforation; various tis- sues have been used for graft material but that in most common use is autologous temporalis fascia, which is taken from just above the patient’s ear. Success rates for this
procedure are very
high.
‘Bony’ CSOM or cholesteatoma
The bone affected by this type of CSOM comprises the tympanic ring, the ossicles, the mastoid air cells and the bony walls of the attic and antrum. The perforation is often postero-superior (Fig. 9.2) or in the pars flaccida (Schrapnell’s membrane) (Fig. 9.3). The discharge is often scanty but usually persistent, and may be foul smelling.
There are other features of this type of CSOM:
• granulations as a result of osteitis;
• aural polyps formed of granulation tissue, which may fill the meatus;
• cholesteatoma.
Cholesteatoma is formed by squamous epithelium within the middle ear. It results in accumulation of keratotic debris. This will be visible through the perforation as keratin flakes, which are white and smelly. The cholesteatoma expands and dam- ages vital structures, such as dura, the facial nerve and the semicircular canals. Cho- lesteatoma is destructive and potentially lethal if
There are other features of this type of CSOM:
• granulations as a result of osteitis;
• aural polyps formed of granulation tissue, which may fill the meatus;
• cholesteatoma.
Cholesteatoma is formed by squamous epithelium within the middle ear. It results in accumulation of keratotic debris. This will be visible through the perforation as keratin flakes, which are white and smelly. The cholesteatoma expands and dam- ages vital structures, such as dura, the facial nerve and the semicircular canals. Cho- lesteatoma is destructive and potentially lethal if
untreated.
Treatment of bony-type CSOM
Regular aural toilet in early cases of mild osteitis may be adequate to prevent progression, but such a case should be watched closely.
Suction toilet under the microscope may evacuate a small pocket of cholesteatoma.
Mastoidectomy is nearly always necessary in established cholesteatoma. This is a major operation to open the mastoid cells, removing cholesteatoma and diseased tissue in the middle ear and mastoid (Fig. 9.4).
Suction toilet under the microscope may evacuate a small pocket of cholesteatoma.
Mastoidectomy is nearly always necessary in established cholesteatoma. This is a major operation to open the mastoid cells, removing cholesteatoma and diseased tissue in the middle ear and mastoid (Fig. 9.4).
Treatment of chronic otitis media
Dry perforation, with no cholesteatoma can be left alone.
Discharge can be managed with topical treatment.
Persistent perforation can be repaired (myringoplasty).
Cholesteatoma needs surgery.
Complications (e.g. spread of infection beyond the ear) need urgent treatment.
Discharge can be managed with topical treatment.
Persistent perforation can be repaired (myringoplasty).
Cholesteatoma needs surgery.
Complications (e.g. spread of infection beyond the ear) need urgent treatment.








اچھی پوسٹ اردو ناول
ردحذف